Not appointed with one of the carriers below
Click the button above to request a contract

Medicare
Supplement Tools

To Access, these files Email is – [email protected]
To Access, these files password is: MEDICARE
Click on the file icon to Access Medicare Supplement Underwriting Documents.
Seniors Choice Group Retiree Medical Plans
Merchants Benefit Administration Seniors Choice Admin 18700 N. Hayden Rd, STE 390 Scottsdale, AZ 85255
Online: www.mbaadmin.com Fax: (480) 776-5054
E-Mail: [email protected]
Questions: (480) 776-5040 (toll-free)
2025 Download NJ Horizon Apps
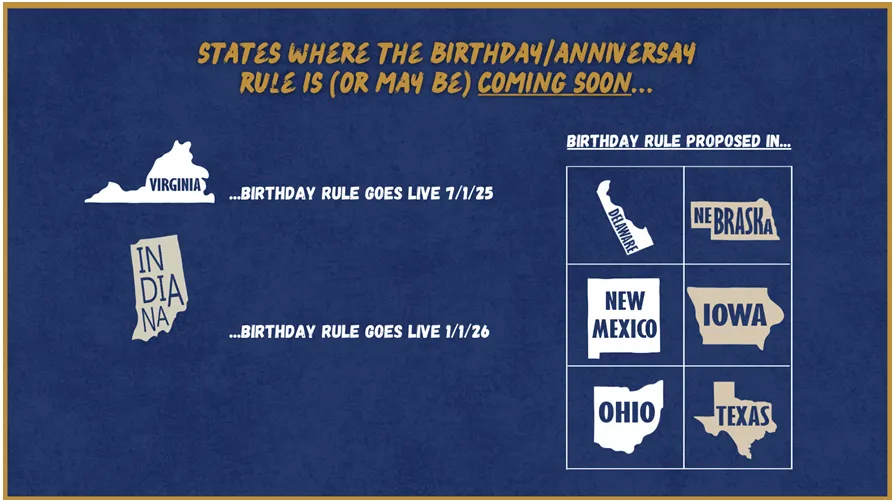
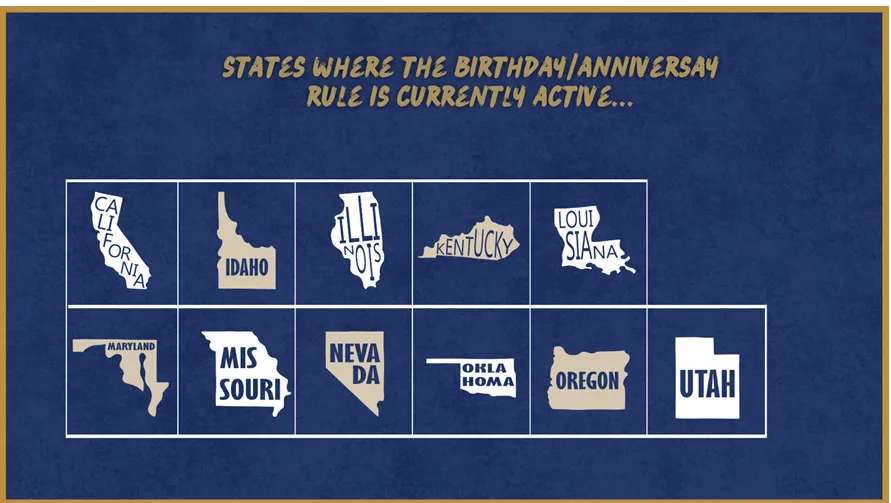
Birthday Rules
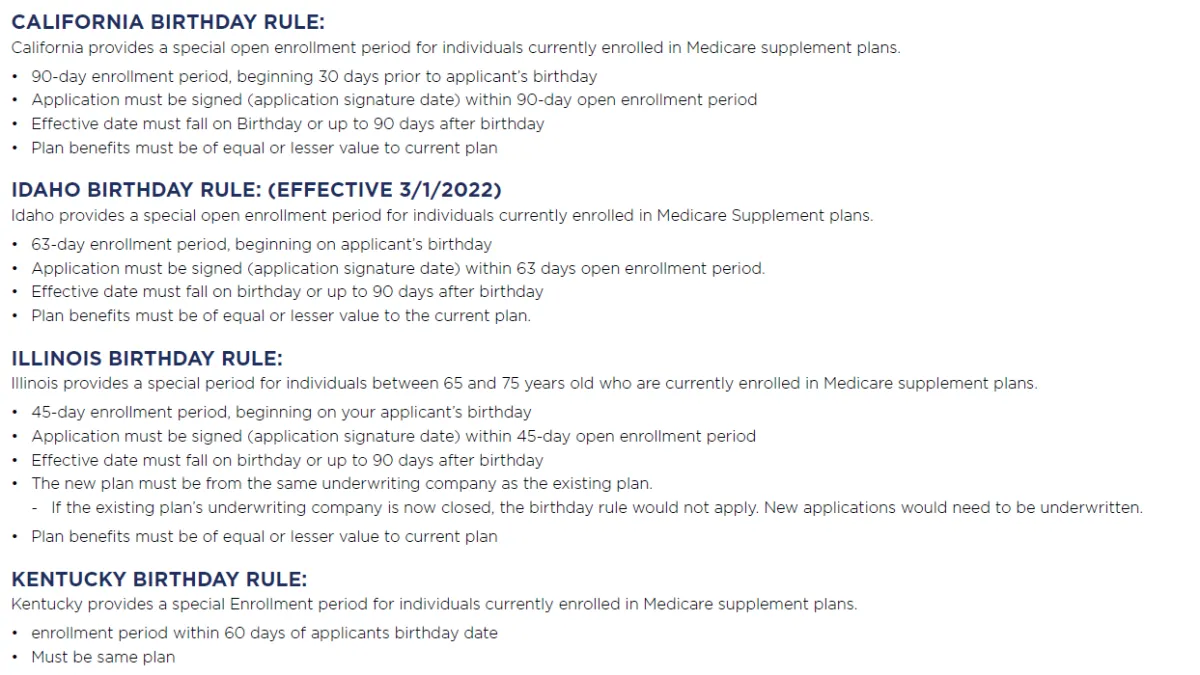
CALIFORNIA BIRTHDAY RULE:
California provides a special open enrollment period for individuals currently enrolled in Medicare supplement plans.
90-day enrollment period, beginning 30 days prior to applicant’s birthday ·
Application must be signed (application signature date) within 90-day open enrollment period ·
Effective date must fall on Birthday or up to 90 days after birthday ·
Plan benefits must be of equal or lesser value to current plan
IDAHO BIRTHDAY RULE:
Idaho provides a special open enrollment period for individuals currently enrolled in Medicare Supplement plans.
63-day enrollment period, beginning on applicant’s birthday ·
Application must be signed (application signature date) within 63 days open enrollment period.
Effective date must fall on birthday or up to 90 days after birthday
Plan benefits must be of equal or lesser value to the current plan.
ILLINOIS BIRTHDAY RULE:
Illinois provides a special period for individuals between 65 and 75 years old who are currently enrolled in Medicare supplement plans.
45-day enrollment period, beginning on your applicant’s birthday ·
Application must be signed (application signature date) within 45-day open enrollment period ·
Effective date must fall on birthday or up to 90 days after birthday
The new plan must be from the same underwriting company as the existing plan.
If the existing plan’s underwriting company is now closed, the birthday rule would not apply.
New applications would need to be underwritten.
Plan benefits must be of equal or lesser value to current plan
KENTUCKY BIRTHDAY RULE (Effective 1/1/24):
Must already have a Medicare Supplement plan.
Must switch to a like plan (example: Plan G to Plan G).
Can apply as early as 30 days before your birthday but no later than 60 days after your birthday.
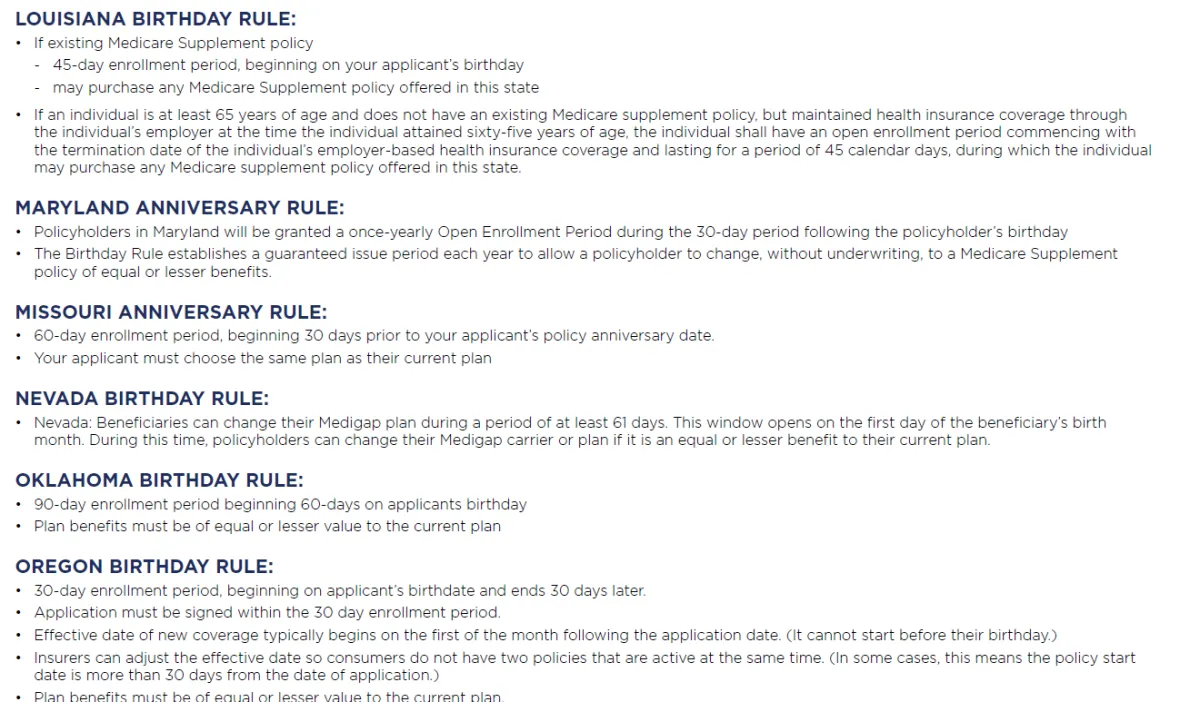
LOUISIANA BIRTHDAY RULE:
If existing Medicare Supplement policy
45-day enrollment period, beginning on your applicant’s birthday
may purchase any Medicare Supplement policy offered in this state
If an individual is at least 65 years of age and does not have an existing Medicare supplement policy, but maintained health insurance coverage through the individual’s employer at the time the individual attained sixty-five years of age, the individual shall have an open enrollment period commencing with the termination date of the individual’s employer-based health insurance coverage and lasting for a period of 45 calendar days, during which the individual may purchase any Medicare supplement policy offered in this state.
MARYLAND ANNIVERSARY RULE:
Policyholders in Maryland will be granted a once-yearly Open Enrollment Period during the 30-day period following the policyholder’s birthday · The Birthday Rule establishes a guaranteed issue period each year to allow a policyholder to change, without underwriting, to a Medicare Supplement policy of equal or lesser benefits.
MISSOURI ANNIVERSARY RULE:
60-day enrollment period, beginning 30 days prior to your applicant’s policy anniversary date.
Your applicant must choose the same plan as their current plan
NEVADA BIRTHDAY RULE:
Nevada: Beneficiaries can change their Medigap plan during a period of at least 61 days.
This window opens on the first day of the beneficiary’s birth month. During this time, policyholders can change their Medigap carrier or plan if it is an equal or lesser benefit to their current plan.
OKLAHOMA BIRTHDAY RULE:
60-day enrollment period beginning on applicants birthday. ·
Individual must be enrolled in a Medicare Supplement plan, with no gap in coverage greater than 90 days since initial enrollment. ·
Plan benefits must be of equal or lesser value to the current plan.
OREGON BIRTHDAY RULE:
30-day enrollment period, beginning on applicant’s birthdate and ends 30 days later.
Application must be signed within the 30 day enrollment period. ·
Effective date of new coverage typically begins on the first of the month following the application date. (It cannot start before their birthday.) · Insurers can adjust the effective date so consumers do not have two policies that are active at the same time. (In some cases, this means the policy start date is more than 30 days from the date of application.)
Plan benefits must be of equal or lesser value to the current plan.
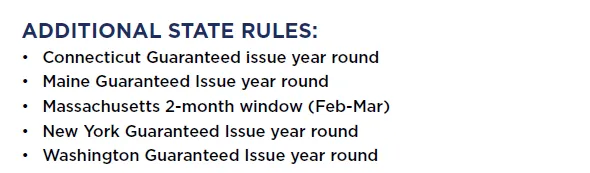
ADDITIONAL STATE RULES:
Connecticut Guaranteed issue year round
Maine Guaranteed Issue year round
Massachusetts 2-month window (Feb-Mar)
New York Guaranteed Issue year round
Washington Guaranteed Issue year round
Frequently asked questions
Can you be denied a Medicare Supplement plan?
If you are in a Medigap enrollment period (6mos of Part B Effective Date) or have the protections of guaranteed issue, your application to enroll in a Medicare Supplement plan can't be denied.
However, outside of these situations, you will have to go through medical underwriting when applying for Medigap, and your application may be denied because of a preexisting health condition, your age or other risk factors.
What's the difference between open enrollment and guaranteed issue?
These two terms are often used interchangeably because guaranteed issue protection (when you can't be denied coverage) happens during open enrollment (the window when you can sign up for plans).
However, the protections of guaranteed issue can also occur outside of open enrollment, allowing you to enroll in a Medigap plan or switch your coverage if you meet the guaranteed issue criteria.
Open enrollment pays a commission while generally gurantee issue does not.
What are the states with the best Medigap guaranteed issue protections?
There are 12 states that provide guaranteed issue protections at least once per year to switch to Medigap or change Medigap plans: California, Connecticut, Idaho, Illinois, Maine, Massachusetts, Missouri, Nevada, New York, Oregon, Rhode Island and Washington.
Medical Questions & Underwriting Guides


Medico
800-748-0026
ACE Medsupp
800-601-3372
Aflac
800-504-0336
Bankers Fidelity
866-458-7501
Cigna MedSupp
877-454-0923
Horizon BCBS of NJ
800-365-2223
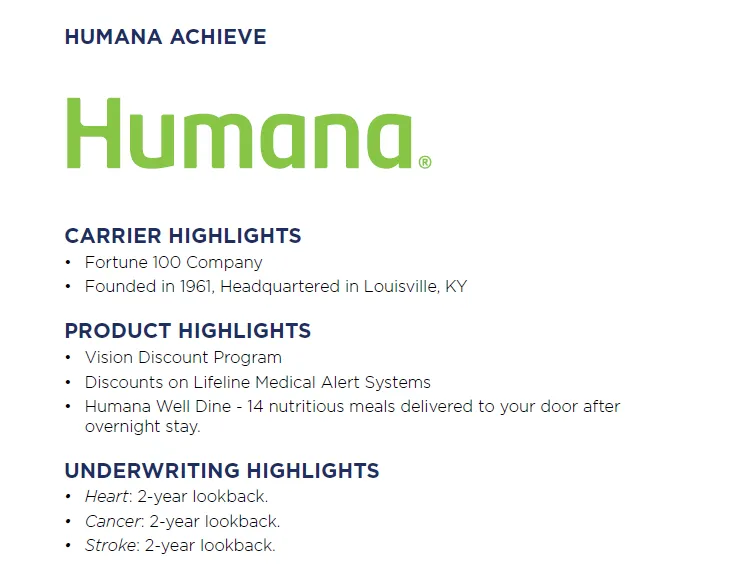
Humana
800-309-3163
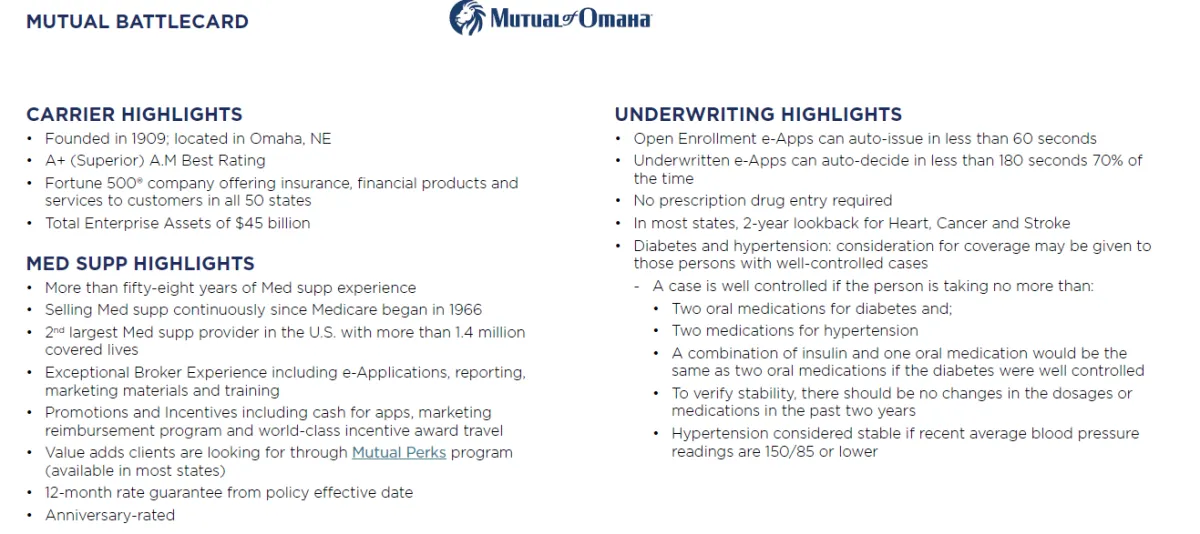
Mutual Of Omaha
800-693-6083
AARP
888-381-8581
AllState Health Solutions
888-966-2345
Aetna Senior Products
866-272-6630
American Benefit Life
1-833-504-0331
Americo
877-212-2346
Anthem
800-633-4368
BCBS of Nebraska
844-201-0763
BCBS of Tennessee
800-565-9140
Blue Shield - California
800-559-5905
Capitol Life
866-237-3010
Central State Health and Life of Omaha
833-522-4874
GPM Life
866-453-4993
Guarantee Trust and Life
800-635-1993
Heartland National
888-996-1619
Liberty Bankers Life
844-770-2400
Manhattan Life
800-877-7703
New Era Life
800-552-7879
Royal Arcanum
888-352- 5158
Sbli | Prosperity eApp
855-321-2755
Sbli | Prosperity agent portal
866-322-2856
Seniors Choice
888-725-3655
Union Security Insurance Company
855-741-4308
United American
800-925-7355
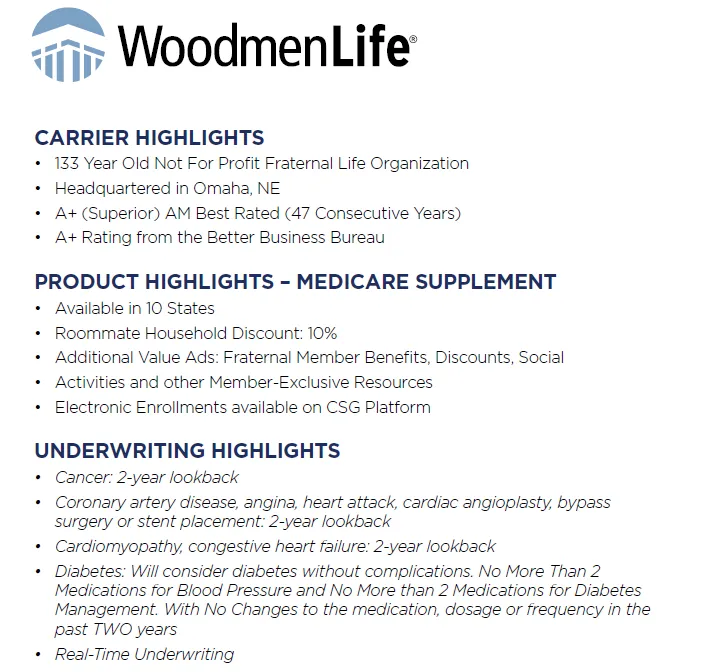
Woodmen Life
1-800-893-6517
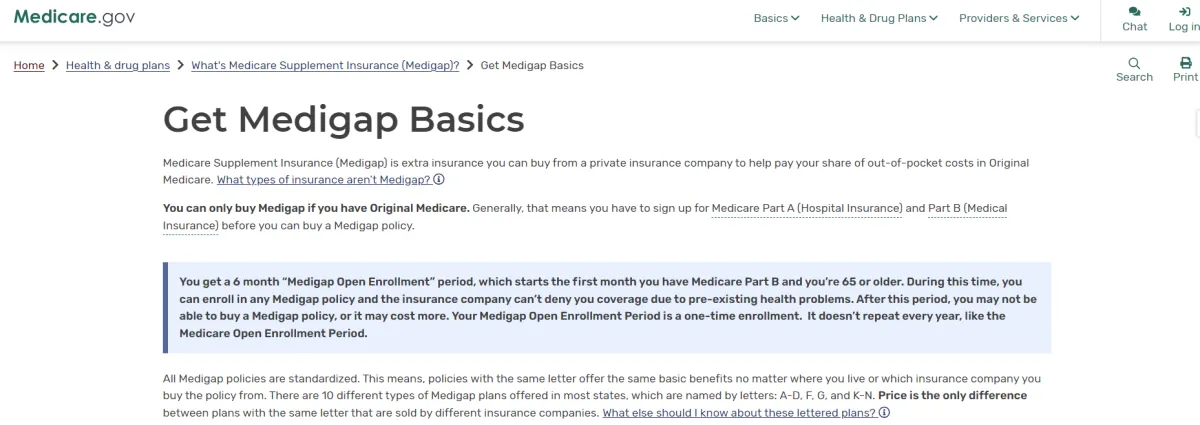
Medigap Open Enrollment:
The best time to buy a Medigap policy is during your 6-month Medigap Open Enrollment Period. This runs from the date you receive Medicare Part B.
During that time you can buy any Medigap policy sold in your state, even if you have health problems. This period automatically starts the first month you have Medicare Part B (Medical Insurance) and you're 65 or older. It can't be changed or repeated.
After this enrollment period, you may not be able to buy a Medigap policy.
After having 6 months of Part B you wll have to qualify and be underwritten to ensure you receive a commission.,
https://www.medicare.gov/supplements-other-insurance/when-can-i-buy-medigap
Guaranteed Issue Rights (Also Called "Medigap Protections")
Typically most insurance carriers do knot pay us a commission if you enroll a client Guarantee Issue Rights.
https://www.medicare.gov/supplements-other-insurance/when-can-i-buy-medigap/guaranteed-issue-rights
are rights you have in certain situations when insurance companies must offer you certain Medigap policies. In these situations, an insurance company:
Must sell you a Medigap policy Must cover all your pre-existing health conditions Can't charge you more for a Medigap policy because of past or present health problems
In most cases, you have a guaranteed issue right when you have other health coverage that changes in some way, like when you lose the other health coverage. In other cases, you have a "trial right" to try a Medicare Advantage Plan (Part C) and still buy a Medigap policy if you change your mind.
You have a guaranteed issue right (which means an insurance company can’t refuse to sell you a Medigap policy) in these situations:
You’re in a Medicare Advantage Plan, and your plan is leaving Medicare or stops giving care in your area, or you move out of the plan's service area.
You have Original Medicare and an employer group health plan (including retiree or COBRA coverage) or union coverage that pays after Medicare pays and that plan is ending.
You have Original Medicare and a Medicare SELECT policy. You move out of the Medicare SELECT policy's service area.
You joined a Medicare Advantage Plan or Program of All-inclusive Care for the Elderly (PACE) when you were first eligible for Medicare Part A at 65, and within the first year of joining, you decide you want to switch to Original Medicare. (Trial Right)
You dropped a Medigap policy to join a Medicare Advantage Plan (or to switch to a Medicare SELECT policy) for the first time, you’ve been in the plan less than a year, and you want to switch back. (Trial Right) Your Medigap insurance company goes bankrupt and you lose your coverage, or your Medigap policy coverage otherwise ends through no fault of your own.
You leave a Medicare Advantage Plan or drop a Medigap policy because the company hasn't followed the rules, or it misled you.
Note
There may be times when more than one of the situations above applies to you. When this happens, you can choose the guaranteed issue right that gives you the best choice.
Access DropBox for Med Supp Underwriting Documents
Email: [email protected]
Password is: MEDICARE
Click on the file icon to Access Medicare Supplement Underwriting Documents.
Sign Your Client up for an AARP membership
Medicare Advantage Enrollment Links
Specializing in Medicare and Senior Products
Long Term Care, Annuities, & Life Insurance
Dental & Vision Plans
Address
Golden Years Design Benefits Inc.
55 Schanck Road Suite A-14
Freehold, NJ 07728
Specializing in Medicare and Senior Products
Long Term Care, Annuities, & Life Insurance
Dental & Vision Plans
Address
Golden Years Design Benefits Inc.
55 Schanck Road Suite A-14










